Glaucoma/ 青光眼
What is Glaucoma?
Glaucoma is a group of diseases that damage the optic nerve and can result in irreversible vision loss and blindness. Glaucoma is one of the leading causes of blindness for people over the age of 60. Oftentimes, a person may have glaucoma without even knowing it, because symptoms do not typically begin to develop until severe damage has already occurred. This is the reasons why we strongly recommend people to see their eye doctor on a regular basis as they age. Glaucoma is often associated with higher eye pressure, but the monitoring of the optic nerve and preventing further nerve damage is the goal of glaucoma treatment. With early detection and treatment, we can often protect your eyes against serious vision loss.
The optic nerve
The optic nerve is a bundle of more than 1 million nerve fibers. It connects the retina to the brain. The retina is the light-sensitive tissue at the back of the eye. A healthy optic nerve is necessary for good vision.
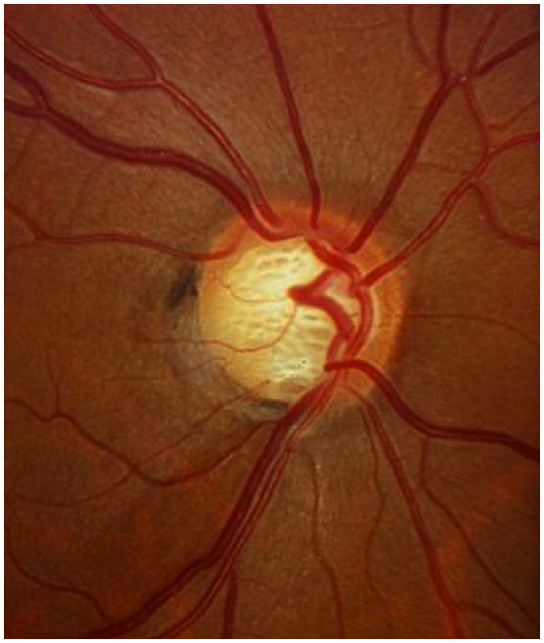
Normal Optic Nerve
Glaucomatous Optic Nerve- loss especially of inferior nerve fibers
How does the optic nerve get damaged by open-angle glaucoma?
Several large studies have shown that eye pressure is a major risk factor for optic nerve damage. In the front of the eye is a space called the anterior chamber. A clear fluid flows continuously in and out of the chamber and nourishes nearby tissues. The fluid leaves the chamber at the open angle where the cornea and iris meet. When the fluid reaches the angle, it flows out of the eye through a spongy layer, called the trabecular meshwork.
In open-angle glaucoma, even though the drainage angle is "open", the fluid passes too slowly through the meshwork drain. As the fluid builds up, the pressure inside the eye rises to a level that may damage the optic nerve. When the optic nerve is damaged from increased pressure, open-angle glaucoma-and vision loss—may result. That’s why controlling pressure inside the eye is important.
Another risk factor for optic nerve damage relates to blood pressure. Thus, it is important to also make sure that your blood pressure is at a proper level for your body by working with your medical doctor.
Do I have glaucoma if I have increased eye pressure?
Not necessarily. Not every person with increased eye pressure will develop glaucoma. Some people can tolerate higher levels of eye pressure better than others. Also, a certain level of eye pressure may be high for one person but normal for another.
Whether you develop glaucoma depends on the level of pressure your optic nerve can tolerate without being damaged. This level is different for each person. That’s why a comprehensive dilated eye exam is very important. It can help your eye care professional to determine what level of eye pressure is normal for you.
Can I develop glaucoma without an increase in my eye pressure?
Yes. Glaucoma can develop without increased eye pressure. This form of glaucoma is called low-tension or normal-tension glaucoma. It is a type of open-angle glaucoma.
Who is at risk for open-angle glaucoma?
Anyone can develop glaucoma. Some people, listed below, are at higher risk than others:
African Americans over age 40
Everyone over age 60, especially Mexican Americans
People with a family history of glaucoma
A comprehensive dilated eye exam can reveal more risk factors, such as high eye pressure, thinness of the cornea, and abnormal optic nerve anatomy. In some people with certain combinations of these high-risk factors, medicines in the form of eyedrops can help reduce the risk of developing glaucoma.
Glaucoma Symptoms
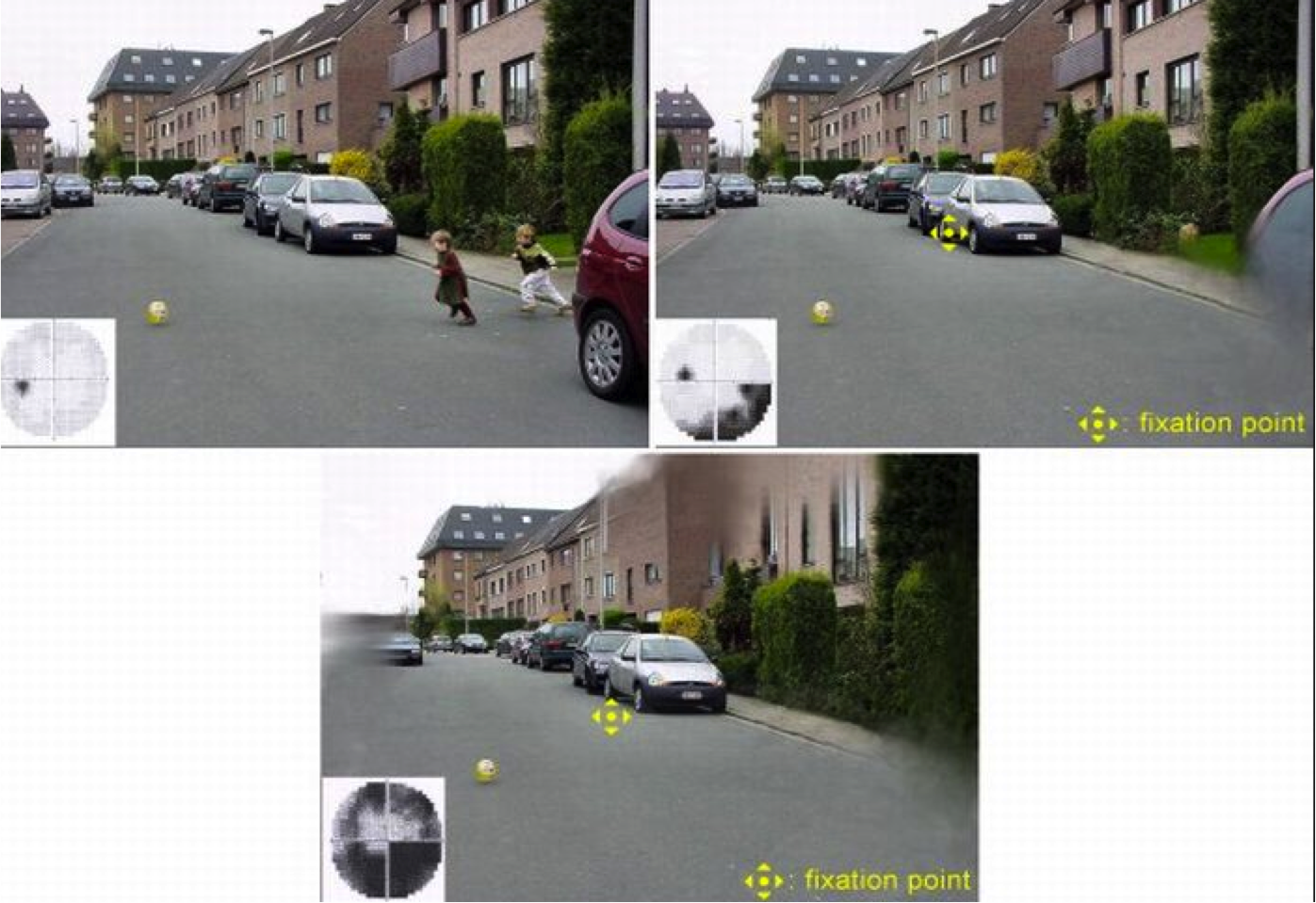
At first, open-angle glaucoma has no symptoms. It causes no pain. Vision stays normal. Glaucoma can develop in one or both eyes. Without treatment, people with glaucoma will slowly lose their peripheral (side) vision. As glaucoma remains untreated, people may miss objects to the side and out of the corner of their eye. They seem to be looking through a tunnel. Over time, straight-ahead (central) vision may decrease until no vision remains.
With Optic nerve damage, the peripheral field is gradually lost first then central vision.
How is glaucoma detected?
Glaucoma is detected through a comprehensive dilated eye exam that includes the following:
Visual acuity test. This eye chart test measures how well you see at various distances.
Visual field test. This test measures your peripheral (side vision). It helps your eye care professional tell if you have lost peripheral vision, a sign of glaucoma.
Dilated eye exam. In this exam, drops are placed in your eyes to widen, or dilate, the pupils. Your eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of damage and other eye problems. After the exam, your close-up vision may remain blurred for several hours.
Tonometry is the measurement of pressure inside the eye by using an instrument called a tonometer. Numbing drops may be applied to your eye for this test. A tonometer measures pressure inside the eye to detect glaucoma.
Pachymetry is the measurement of the thickness of your cornea. Your eye care professional applies a numbing drop to your eye and uses an ultrasonic wave instrument to measure the thickness of your cornea.
Can glaucoma be cured?
No. There is no cure for glaucoma. Vision lost from the disease cannot be restored.
Glaucoma Treatments
Immediate treatment for early-stage, open-angle glaucoma can delay progression of the disease and prevent vision loss. That’s why early diagnosis is very important. Glaucoma treatments include medicines, laser trabeculoplasty, conventional surgery, or a combination of any of these. While these treatments may save remaining vision, they do not improve sight already lost from glaucoma. When it comes to treating glaucoma, Dr. Lee, can help you understand the different options you have to choose from. Some options may be more suited to your condition, while others may not. Dr. Lee will recommend the best choices for you based off of the current stage of your disease, and your overall health in general.
Medicines. Medicines, in the form of eyedrops or pills, are the most common early treatment for glaucoma. Taken regularly, these eyedrops lower eye pressure. Some medicines cause the eye to make less fluid. Others lower pressure by helping more fluid drain from the eye. Many medicines are available to treat glaucoma. Most people have no problems. However, some medicines can cause side effects. For example, drops may cause stinging, burning, and redness in the eyes. If you have problems with one medicine, tell your eye care professional. Treatment with a different dose or a new medicine may be possible.
Because glaucoma often has no symptoms, people may be tempted to stop taking, or may forget to take their medicine. Glaucoma medicines need to be taken regularly and continued as long as they help control your eye pressure.
Selective laser trabeculoplasty (SLT). Selective Laser Trabeculoplasty is a form of laser surgery that is used to lower intraocular pressure in glaucoma. This is done by applying laser energy to the drainage tissue in the eye. This causes both a chemical and biological change that results in better drainage of fluid out of the eye. This eventually results in lowering of IOP by about 30% when used as initial therapy. This is roughly equal to using one glaucoma medication. The effects typically take 6-8 weeks to appear, and usually last between 1-5 years. If it does not last at least 6-12 months, it is usually not considered successful. The procedure can be repeated if the effect wears off over time. Repeat treatments may or may not lower IOP as much as the first, and continued repeat lasering will eventually not be effective. Some patients can be controlled with just laser treatment. Others require additional IOP lowering and may therefore need to use glaucoma medication as well. Risks include post-operative inflammation and a 5% incidence of IOP elevation after laser. This can be managed with glaucoma medications and usually goes away after 24 hours.
Incisional glaucoma surgery.
Trabeculectomy. A trabeculectomy is a surgical procedure that reduces the buildup of intraocular eye pressure (IOP) in the eye. It is performed by creating a small hole in the wall of the eye, just directly above the iris, to allow more fluid to flow out of the eye. This aqueous fluid will drain and collect inside a small blister-like reservoir called a bleb, located superiorly, just under the upper eyelid.
This surgery is normally done as an outpatient procedure, usually taking about an hour to perform. Most patients are able to return home the very same day. Complete healing usually takes up to 3 months, and during this time, the vision can fluctuate.
Trabeculectomy is about 70 to 90 percent effective at lowering eye pressure. If the new drainage opening narrows, a second operation may be needed. This surgery works best in eyes without previous eye surgery.
Over time, the surgical hole may close and the pressure can rise again. This is due to the body trying to heal. This healing response is stronger and occurs most often in younger people, because they have a stronger healing response. The use of drugs, such as mitomycin-C and 5-FU, at the time of surgery, can help to slow down the healing of the opening.
Tube shunt surgery. This is another glaucoma surgery that focuses on allowing better drainage of fluid from the eye. It involves the placement of a small, soft tube into the eye. The small tube shunt allows the drainage of aqueous fluid out of the eye, collecting into a small silicone pouch, resting on the superior surface of the eyeball, and is covered by the eyelid. This collection of fluid is then absorbed by the eye veins and carried away into the blood circulation.
What are some other forms of glaucoma and how are they treated?
Open-angle glaucoma is the most common form. Some people have other types of the disease.
In low-tension or normal-tension glaucoma, optic nerve damage and narrowed side vision occur in people with normal eye pressure. Lowering eye pressure at least 30 percent through medicines slows the disease in some people. Glaucoma may worsen in others despite low pressures. A comprehensive medical history is important to identify other potential risk factors, such as low blood pressure, that contribute to low-tension glaucoma. If no risk factors are identified, the treatment options for low-tension glaucoma are the same as for open-angle glaucoma.
In angle-closure glaucoma, the fluid at the front of the eye cannot drain through the angle and leave the eye. The angle gets blocked by the iris. People with this type of glaucoma may have a sudden increase in eye pressure. Symptoms include severe pain and nausea, as well as redness of the eye and blurred vision. If you have these symptoms, you need to seek treatment immediately. This is a medical emergency. If your doctor is unavailable, go to the nearest hospital or clinic. Without treatment to restore the flow of fluid, the eye can become blind. Usually, prompt laser surgery and medicines can clear the blockage, lower eye pressure, and protect vision.
In congenital glaucoma, children are born with a defect in the angle of the eye that slows the normal drainage of fluid. These children usually have obvious symptoms, such as cloudy eyes, sensitivity to light, and excessive tearing. Conventional surgery typically is the suggested treatment, because medicines are not effective and can cause more serious side effects in infants and be difficult to administer. If surgery is done promptly, these children usually have an excellent chance of having good vision.
Secondary glaucomas can develop as complications of other medical conditions. For example, a severe form of glaucoma is called neovascular glaucoma, and can result from poorly controlled diabetes or high blood pressure. Other types of glaucoma sometimes occur with cataract, certain eye tumors, or when the eye is inflamed or irritated by a condition called uveitis. Sometimes glaucoma develops after other eye surgeries or serious eye injuries. Steroid drugs used to treat eye inflammations and other diseases can trigger glaucoma in some people. There are two eye conditions known to cause secondary forms of glaucoma. Pigmentary glaucoma occurs when pigment from the iris sheds off and blocks the meshwork, slowing fluid drainage. Pseudoexfoliation glaucoma occurs when extra material is produced and shed off internal eye structures and blocks the meshwork, again slowing fluid drainage.
Depending on the cause of these secondary glaucomas, treatment includes medicines, laser surgery, or conventional or other glaucoma surgery.
What You Can Do
If you are being treated for glaucoma, be sure to take your glaucoma medicine every day. See your eye care professional regularly. If you are unsure whether you have glaucoma or not, or if you are unsure whether your glaucoma is under adequate control, call to make an appointment to see Dr. Lee. Dr. Lee is a fellowship trained glaucoma specialist with over a decade of experience. He is able to manage your glaucoma using the latest treatment options (including medications, laser, and surgery).
You also can help protect the vision of family members and friends who may be at high risk for glaucoma-African Americans over age 40; everyone over age 60, especially Mexican Americans; and people with a family history of the disease. Encourage them to have a comprehensive dilated eye exam once every year. Remember that lowering eye pressure in the early stages of glaucoma slows progression of the disease and helps save vision.
Courtesy of NEI-Glaucoma